Introduction
Melanoma is a form of skin cancer that can be deadly due to its metastatic nature. More advanced cases of melanoma can invade the lymph nodes and surrounding organs, causing secondary cancers, such as breast cancer. When melanoma cancer cells are able to invade the surrounding tissues, lymph nodes, and lymph fluid, the risk of developing breast or other types of cancer increase significantly.
In this article, we will examine the causes of melanoma and those patients who may be at risk of developing secondary cancers, such as breast cancer. We will also examine how a breast cancer diagnosis may affect the risk of developing melanoma.
Melanoma
A diagnosis of melanoma can occur when the skin has been exposed to volumes of UV radiation the body cannot tolerate. UV radiation attacks the DNA in the skin cells and causes them to mutate. These mutations become cancerous when the body’s immune system can not repair the damage.
While UV radiation from the sun, tanning beds, UV lights, etc., are the primary cause of melanoma, family history also plays a role. According to Cancer.net, 8% of newly diagnosed melanoma patients have a parent or sibling with the disease. However, everyone is at risk of developing skin cancer sometime during their lifetime.
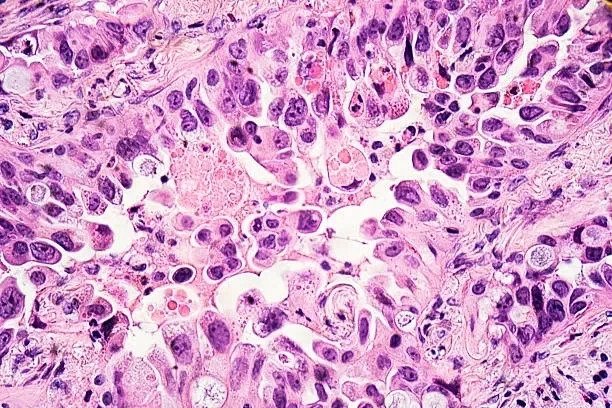
Metastatic Melanoma
When detected early, some stages of melanoma are easily treated with surgery or medications. When your dermatologist finds a spot that is suspicious for melanoma, he or she will perform a biopsy to analyze the cells and understand the depth of the tumor, known as the Breslow thickness. Biopsies that are positive for melanoma cells with a Breslow thickness of less than 0.8 mm are generally easy to treat. This means the melanoma tumor, or superficial melanoma, is less than 0.8 mm deep into the skin.
Melanoma biopsies from 0.8 mm up to 1.0 mm Breslow thickness are considered thin melanomas, are often treated with Mohs surgery or excisions, and may or may not require more complex follow-up. Your dermatologist will review your family history and risk scores to determine if additional specialists and testing are required.
Breslow-thickness melanoma tumors greater than 1.0 mm in depth are considered more concerning, and your dermatologist may recommend body scans and sentinel lymph node biopsies to determine potential metastasis. In patients with lymph node biopsies positive for melanoma cells, the risk of developing secondary cancers, such as breast cancer, rises.
The Role of Lymph Nodes
Lymph nodes are small “glands” that are part of the immune system. They are filters for the body and help fight diseases and infections. Lymph nodes transport fluid throughout the body, destroying harmful substances and transporting them safely out of the body through the kidneys or bowel.
Metastasis to lymph nodes and surrounding tissues or organs can occur when the number of melanoma cancer cells overwhelms the lymph system. The weakened lymph nodes can no longer destroy the cancer cells; the lymph fluid carries melanoma cells throughout the body. This means tissues, organs, or other structures in close proximity to the lymph nodes and lymph fluid are at risk of invasion from the cancer cells. This is how a secondary cancer diagnosis, like breast cancer, can arise from a melanoma tumor.
Breast Cancer Risk with a Melanoma Diagnosis
According to the Journal of the American Academy of Dermatology, a melanoma tumor can become a “donor tumor” and be the primary cause of a secondary breast cancer diagnosis. The Ochsner Journal in the National Library of Medicine documents a case study where a 1.1 mm Breslow thickness melanoma tumor metastasized to the patient’s breasts four (4) years after removing and treating her primary melanoma tumor. This link between donor tumor and secondary cancer diagnosis has been well studied, with over 360 clinical trials conducted between 1999 and today.
In fact, patients with melanoma have a 1.4 times greater risk of developing breast cancer. Interestingly, the metastasis risk is bi-directional. Due to the gene similarity between melanoma and breast cancer, those patients with primary breast cancer have a 2.5 times greater risk of developing melanoma in their lifetime.
Prevention and Early Detection are the Key
Prevention and early detection are the best ways to avoid primary melanoma and metastasis. Prevention of melanoma consists of the following:
- Protecting your skin from UV rays with sunscreen or sunblock clothing
- Avoiding high UV radiation hours of the day (10 am to 4 pm in the US)
- Refraining from the use of tanning beds or UV lights
- Yearly or more frequent full-body skin exams as recommended by your dermatologist
Self-skin exams for the ABCDE of Melanoma:
- A – Asymmetry – one side of the lesion is different from the other side
- B – Border – an irregularly shaped border
- C – Color – varying color or darkening of a lesion
- D – Diameter – a lesion larger than a pencil eraser
- E – Evolving – growing or changing of the lesion over time
If you have a history of melanoma, make sure to tell your family doctor, oncologist, gynecologist, or other trusted healthcare provider. Discuss the mammogram frequency that makes the most sense for you. Conversely, if you have a history of breast cancer, make sure to share this information with your dermatologist. Because melanoma and breast cancer metastasis can be bi-directional (move in either direction), surveillance for both diseases is vital to your overall health.
Please visit the American Cancer Society for more information about the links between melanoma and breast cancer. For more information on melanoma and other forms of skin cancer, please visit the American Academy of Dermatology Association.
Disclaimer: The information provided in this article is intended to raise awareness and educate the public. It is not intended to be a substitute for diagnosis and treatment. If you have health concerns, please visit your healthcare provider.